Date: 7 February 2014
Copyright: n/a
Notes:
Patient JS (age 53) has chronic cavitary pulmonary aspergillosis and failed itraconazole therapy. After taking voriconazole for several months she relatively suddenly developed florid conjunctivitis which is attributable to voriconazole. This occurred without facial erythema, which is unusual. Voriconazole has been continued.
Images library
-
Title
Legend
-
X-Rays -Allergic Bronchopulmonary Aspergillosis (ABPA) with 3 relapses.
A female patient JO (50 yrs) with right middle lobe collapse. The patient presented with a 6 month history of cough which has persisted despite antibiotics and both steroid and salbutamol inhalers. She then developed acute breathlessness with coughing and wheezing. There was no history of asthma. Bronchoscopy (Image K) showed a mucous plug obstructing the right upper lobe bronchus.
Images D – G are X rays showing relapse in 1998 and recovery
Images H – J are X rays showing relapse in 2003
Image K. Bronchoscopy appearance of mucous impaction of the bronchus intermedius – pt JO (50yrs). There was a long mucous plug in the anterior segment of the RUL. Half of this was aspirated and sent for microscopy and culture. The second half “fell into” the bronchus intermedius (which feeds the right middle lobe) and was only partially aspirated.
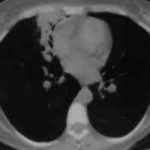
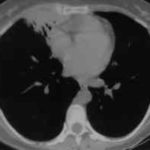
Images L – O: High resolution CT scan of thorax in pt JO, post bronchoscopy. 1.5mm sections at 1 cm intervals of whole lung. There is collapse and consolidation in the right middle lobe with dilation of the right middle lobe bronchi. There is also minor bronchiectasis in the right upperlobe with a little patchy air space shadowing . There is no mediastinal lymphadenopathy or any interstitial fibrosis.
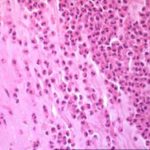
Image P & Q: Histology: Mucous plug (3x 0.5x 0.5cm) containing numerous inflammatory cells, including eosinophils and nuclear debris.GMS staining reveals occasional fungal hyphae with septa and dichotomous branching. These appearances support the diagnosis of bronchopulmonary Aspergillosis. Bronchioalveolar lavage fluid was negative on microscopy and no fungi were grown. A year later Aspergillus fumigatus was grown from her sputum.
 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,