Date: 3 April 2014
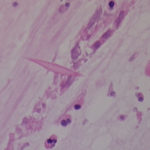
Transmission electron micrograph of a C. neoformans cell seen in CSF in an AIDS patients with remarkably little capsule present. These cells may be mistaken for lymphocytes.
Copyright: n/a
Notes: n/a
Images library
-
Title
Legend
-
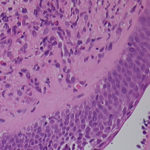
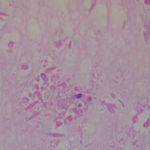
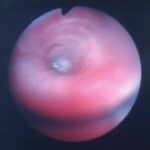
Images EF & G Mucous plug – Stains for fungal elements such as Grocott and PAS revealed no fungal elements. Appearance of specimens is consistent with allergic pulmonary fungal disease.
Despite the lack of fungal elements the histopathology is still indicative of ABPA.
 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
, 
-
Even tilted the sputum barely flowed downhill. This patient was struggling to bring up her sputum, and hypertonic saline (5 mL NaCl 7%) nebulisers twice daily were prescribed with considerable improvement

-
This recording of peak flow was taken prior to and during the first 4 weeks of inhaled steroids (Becotide 100 and Duovent both 2 puffs 4x daily). The patient had had asthma since age 4, and been treated with bronchodilators and oral courses of steroids when severely affected. The chart, which the patient completed at home, shows that early in week one her peak flow varied from 200-250 L/min. As the medication started to work, the peak flows gradually increased to reach 360-420 L/min in the 4th week. The lower value each morning is characteristic of asthma.
The response to steroids is important confirmation of the diagnosis of asthma (reversible airways obstruction). Many years later she developed ABPA, while on inhaled steroids, with severe upper lobe central bronchiectasis, an IgE of 6,800 Kiu/L, positive aspergillus precipitins, an Aspergillus RAST of 58.7KUa/L (normal <0.4) and eosinophilia.

-
Further details
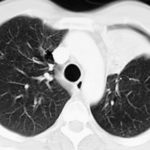
Image A 13/12/66 Asthma. Chest x-ray showing slightly streaky shadowing both bases and left mid and upper zone shadowing, and left apical scarring. The bronchial wall thickening in the left lobe is suspicious of bronchiectasis.
Image B 4/3/69Asthma with bronchiectasis. Chest x-ray showing mild left mid zone shadows consistent with bronchiectasis and a small area of opacification in the left base, with left apical scarring. New streaky shadowing is projected over the left heart border.
Image C 19/10/71 Asthma with bronchiectasis.Chest x-ray showing obliteration of the left aorto-pulmonary window and upper lobe streaking and cavitation and a mid zone small cavitary lesion, most likely a thickened bronchus end on.
Image D 22/9/81 Asthma with bronchiectasis and first radiological clue of ABPA. Chest x-ray showing left upper zone patchy shadowing or atelectasis with obliteration of the left aorto-pulmonary window. There is new right upper lobe streaky shadowing with slight right upper lobe volume loss.
Image E 3/11/81 Asthma with bronchiectasis and first radiological clue of ABPA. Chest x-ray showing clearance of the left upper lobe shadowing after physiotherapy and corticosteroids, compare with X ray D. This clearing with steroids is characteristic of ABPA. However, there is now extensive bronchiectasis in the left lower and right lower lobes.
Image F 17/9/85 Asthma with bronchiectasis and ABPA, with first clue of chronic cavitary pulmonary aspergillosis (CCPA). Chest x-ray showing development of right upper pleural thickening with further volume loss, without extensive fibrotic disease. There is more obvious new cavity formation in the left upper lobe with unchanged thickened bronchi in the left mid zone. A mild scoliosis has developed.
Image G 19/7/93 Asthma with bronchiectasis and ABPA, with now overt chronic cavitary pulmonary aspergillosis (CCPA), bilaterally Chest x-ray showing extensive shadowing at the right base consistent with a chest infection or plugging, ring shadows and coarse markings throughout the lung fields consistent with bronchiectasis and right apical pleural thickening which has progressed. The cavities in the left upper lobe have expanded in size. Her scoliosis has progressed.
Image H 05/06/95 Asthma with bronchiectasis, ABPA and CCPA with possible airway plugging due to ABPA. Chest x-ray showing interval development of scoliosis with bilateral upper lobe pleural thickening, worse on the right, with cavities in the left upper lobe and fullness of the right upper mediastinum.
Image I 08/03/99 Asthma with bronchiectasis, ABPA and CCPA with obvious progression of bronchiectasis, and ? ABPA-related collapse left side Chest x-ray showing marked scoliosis, stable mild left upper lobe fibrosis and cavity formation, and stable right upper lobe pleural thickening. Her trachea is newly displaced to the right. There is a rounded peripheral wedge-shaped area in the right upper lobe, possibly sub-segmental collapse. Both cystic and varicose bronchiectasis are seen in the proximal left lower lobe.
Image J 11/10/02 Asthma with bronchiectasis, ABPA and CCPA which has progressed. Chest x-ray ( computed radiography) showing extensive bronchiectasis, with contraction and fibrosis with cavitation of the left apex, right upper pleural thickening also with cavities in the right upper zone. Large cavities are seen immediately to the right of the trachea with a probable fluid level.
Image K 05/04/04 Asthma with bronchiectasis, ABPA and CCPA with large airway disease of uncertain cause. Chest radiograph showing a right apical cavity free of fluid. Possible constriction of the trachea above the carina and also of the proximal left main bronchus, without an obvious extrinsic mass. There is some improvement of the right upper lobe pleural thickening inferiorly. Otherwise other findings are stable.
Image L. Case MD (now aged 67). In late 2005, she deteriorated on itraconazole and was admitted to hospital for antibiotic therapy. Coughing resulted in a rib fracture. Her prednisolone dose was 10mg daily, necessary to control her asthma and respiratory symptoms, but had lead to osteoporosis and an achilles tendon rupture. Her total IgE was 910KIU/L in August 2005, and Aspergillus specific IgE 34.4 KUa/L, lower than some years before. Pseudomonas was being grown continually from her sputum. Her symptoms continued despite antibiotics and it was judged that her ABPA was out of control, and voriconazole 200mg twice daily was substituted, and itraconazole stopped.
Over the following months and years, there was gradual improvement in her chest symptoms. Her prednisolone dose was reduced to 5mg daily, and given in combination with a moderate dose inhaled steroid. Her total IgE fell to 310 KIU/L and Aspergillus specific IgE to 9.0 KUa/L by 2009. Her FEV1 and FVC had remained stable between 1999 and 2010 at 0.95 and 2.04 (pre-salbutamol) and 1.0 and 2.29.
She had one admission for a chest infection requiring antibiotics in 2011. Her walking distance once she had recovered was 150 meters and her FEV1 in 2011 was 0.82. She continued to remain well and at the end of 2014 was still colonised by Pseudomonas, but doing well. Her XR was almost unchanged from 2004. ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
, 






 ,
, 