Date: 26 November 2013
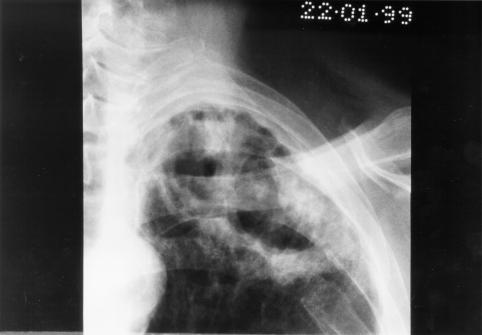
Image A. This man presented with fever and chest pain and was treated with antibiotics. His symptoms partially improved, but slowly. He was 62 years old and had drunk alcohol to excess in the past. He was a smoker. A small infiltrate is seen in the left apex.
Image B. He remained unwell and because the evolution of his chest X-ray was reminiscent of tuberculosis, was transferred to the infectious disease department. Sputum samples were negative for acid fast bacilli (and subsequently culture negative).
Image C. He continued to cough and had low grade fever. His chest X-ray now showed extensive cavitation at the left apex.
Image D. The patient’s symptoms had now resolved. The chest X-ray shows a pair of large thick walled cavities at the left apex. He was on therapy for primary Aspergillus pneumonia (a presumptive diagnosis) with itraconazole 200 mg twice daily.
Image E. A needle biopsy was done which yielded nonspecific chronic inflammatory tissue. He was being treated with itraconazole. Serology now showed one precipitin line to Aspergillus having been negative previously and his IgE was 6000 iu/ml (normal < 150 iu/ml).
Image F. The patient was now asymptomatic on itraconazole (which was given for 6 months). His chest X-ray shows continued resolution of the cavity infiltrate.
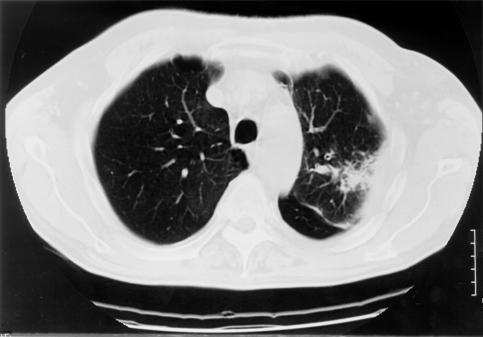
Image G. The CT scans show left apical consolidation with cavitation, with a loose infiltrate inferiorly. The features are consistent with an apical cavitating pneumonia.
Image H. The CT scan shows left apical consolidation with cavitation, with a loose infiltrate inferiorly. The features are consistent with an apical cavitating pneumonia.
Copyright: n/a
Notes: n/a
Images library
-
Title
Legend