Date: 29 August 2017
Copyright:
Fungal Infection Trust
Notes:
ptAS is seen at the National Aspergillosis Centre in Manchester, UK and has ABPA and bronchiectasis
Images library
-
Title
Legend
-
PtDS2 –Repeated chest infections arrested by itraconazole therapy in ABPA and bronchiectasis
DS2 developed asthma age 24 and now aged 62. From about age 30 she started getting repeated chest infections and a few years later ABPA and bronchiectasis was diagnosed. Infections continued requiring multiple courses of antibiotics annually. At one point DS2 developed a pneumothorax, possibly because of excess coughing. She has chronic rhinitis and mannose binding lectin deficiency. In May 2011, she started itraconazole therapy, and has needed no antibiotic courses for her chest since. Her rhinitis with sinusitis occasionally bothers her. She is delighted to have gone 18 months with no chest infections.
 ,
,  ,
, 
-
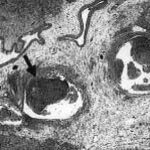
Aspergillus hyphae (arrow) in the lumen without invasion of the necrotic bronchial wall (*) (Nicod 2001).
-
fibrinonecrotic material (arrow) from the airway shown in A, with subocclusion of the bronchial lumen (*)
-
Fibrinous or pseudomembranous bronchitis (arrow) with subocclusion of the airways (* indicates subocclusion of the airways by pseudomembranes)

-
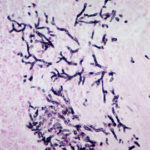
Bronchoscopic biopsy demonstrated septate hyphae with branching at 45o (methenamine silver stain ×400).
-
Bronchoscopic manifestations of Aspergillus tracheobronchitis. (a) Type I. Inflammatory infiltration, mucosa hyperaemia and plaques of pseudomembrane formation in the lumen without obvious airway occlusion. (b) Type II. Deep ulceration of the bronchial wall. (c) Type III. Significant airway occlusion by thick mucous plugs full of Aspergillus without definite deeper tissue invasion. (d) Type IV. Extensive tissue necrosis and pseudomembrane formation in the lumen with airway structures and severe airway occlusion (Wu 2010).








