Date: 26 November 2013
Grocott (silver) stain showing branching septate hyphae fairly typical of Aspergillus in mucus. The apparent right angle branching is unusual.
Copyright:
Fungal Infection Trust
Notes:
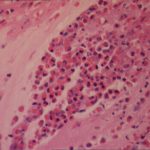
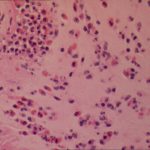
Mucoid impaction due to ABPA- Pt DL.A 57 year old woman presented with breathlessness. She had a history of mild asthma for which she occasionally took salbutamol inhaler puffs. The patient underwent a pneumonectomy because of the severity of her disease process, and uncertainty about the diagnosis, prior to serology results being obtained.Serology showed an IgE of 2600, with a strongly positive Aspergillus RAST test and weakly positive Aspergillus precipitins. Material removed at bronchoscopy showed eosinophilia. These features confirm a diagnosis of allergic bronchopulmonary aspergillosis (ABPA).
Images library
-
Title
Legend
-
Bronchoscopic manifestations of Aspergillus tracheobronchitis. (a) Type I. Inflammatory infiltration, mucosa hyperaemia and plaques of pseudomembrane formation in the lumen without obvious airway occlusion. (b) Type II. Deep ulceration of the bronchial wall. (c) Type III. Significant airway occlusion by thick mucous plugs full of Aspergillus without definite deeper tissue invasion. (d) Type IV. Extensive tissue necrosis and pseudomembrane formation in the lumen with airway structures and severe airway occlusion (Wu 2010).

-
High resolution CT showing centrilobular nodular opacities and branching linear opacities (tree-in-bud appearance) (Al-Alawi 2007).

-
Chest X-ray showing poorly defined bilateral nodular opacities (Al-Alawi 2007).

-
Gross pathologic specimen from autopsy shows the bronchial lumen covered by multiple whitish endobronchial nodules (arrows) (Franquet 2002).

-
Invasive tracheobronchitis showing numerous nodules seen during bronchoscopy (Ronan D’Driscoll).

-
Pseudomembranous seen overlying the bronchial mucosa (Tasci 2006).