Date: 26 November 2013
This recording of peak flow was taken prior to and during the first 4 weeks of inhaled steroids (Becotide 100 and Duovent both 2 puffs 4x daily). The patient had had asthma since age 4, and been treated with bronchodilators and oral courses of steroids when severely affected. The chart, which the patient completed at home, shows that early in week one her peak flow varied from 200-250 L/min. As the medication started to work, the peak flows gradually increased to reach 360-420 L/min in the 4th week. The lower value each morning is characteristic of asthma.
The response to steroids is important confirmation of the diagnosis of asthma (reversible airways obstruction). Many years later she developed ABPA, while on inhaled steroids, with severe upper lobe central bronchiectasis, an IgE of 6,800 Kiu/L, positive aspergillus precipitins, an Aspergillus RAST of 58.7KUa/L (normal <0.4) and eosinophilia.
Copyright: n/a
Notes: n/a
Images library
-
Title
Legend
-
This 24-year-old male with AML on chemotherapy developed recent onset fever and cough. B- Representative section of High Resolution CT shows centri-lobular nodules, ‘tree-in-bud’ appearance consistent with bronchogenic spread of disease.

-
This 24-year-old male with AML on chemotherapy developed recent onset fever and cough. A: Chest radiograph showing patchy air space consolidation involving both lungs.

-
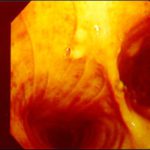
This man with severe chronic fibrosing alveolitis underwent a single left lung transplant at the end of November 2004. Postoperatively he developed reperfusion pulmonary oedema and was difficult to ventilate. He also developed acute renal failure requiring haemodialysis/haemofiltration which corrected his fluid overload and rising creatinine.Rejection was prevented with cyclosporin, mycophenolate and a decreasing dose of methylprednisolone. Cardiovascular problems identified mild pulmonary anastomostic stenosis with a 5% pressure gradient. He had a tracheostomy about 12 days post transplant. He then developed episodes of hypoxia and increased ventilatory pressures. Several bronchoscopies showed mucus plugging in the trachea and major bronchi. These were aspirated, with improvement of oxygenation. Cultures of one of these plugs grew A. fumigatus. These images show a bronchoscopy view of the trachea and anastomosis. Major obstruction of the airway is visible (70%) distal to the anastomosis which looks healthy. Some evidence of tracheal inflammation is visible.
 ,
, 
-
The chest x-ray shows a patient who had a left lung transplanted in May 2003 for cryptogenic fibrosing alveolitis, which was diagnosed post-transplant as sarcoidosis.

-
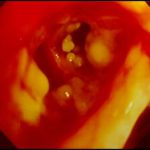
Tracheal aspergillosis. Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.

-
Tracheal aspergillosis, Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.

-
Tracheal aspergillosis. Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.
-
Tracheal aspergillosis. Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.
-
Aspergillus tracheobronchitis in a normal child. This figure, drawn in 1890, illustrates the appearances of the trachea and main bronchi at autopsy in a 3 year old child. She had little else wrong at autopsy other than a minor degree of tuberculosis. She is the first recorded case of Aspergillus tracheobronchitis in the literature and illustrates well that this disease can affect previously well non-inimmunocompromised people. The full case is reported in Wheaton SW.


