Date: 26 November 2013
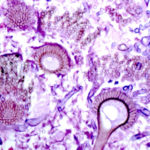
Aspergillus terreus Thom. Conidial head of Aspergillus terreus. Conidial heads are compact, columnar and biseriate. Conidiophores are hyaline to slightly yellow and smooth walled.
Copyright:
With thanks to G Kaminski. D Ellis and R Hermanis Mycology Unit, Women’s & Children’s Hospital , Adelaide, South Australia 5006
Notes:
Colonies on CYA 40-50 mm diam, plane, low and velutinous, usually quite dense; mycelium white; conidial production heavy, brown (Dark Blonde to Camel, 5-6D4); reverse pale to dull brown or yellow brown. Colonies on MEA 40-60 mm diam, similar to those on CYA or less dense. Colonies on G25N 18-22 mm diam, plane or irregularly wrinkled, low and sparse; conidial production light, pale brown; brown soluble pigment sometimes produced; reverse brown. No growth at 5°C. Colonies at 37°C growing very rapidly, 50 mm or more diam, of similar appearance to those on CYA at 25°C.Conidiophores borne from surface hyphae, stipes 100-250 μm long, smooth walled; vesicles 15-20 μm diam, fertile over the upper hemisphere, with densely packed, short, narrow metulae and phialides, both 5-8 μm long; conidia spherical, very small, 1.8-2.5 μm diam, smooth walled, at maturity borne in long, well defined columns.Distinctive featuresVelutinous colonies formed at both 25°C and 37°C, uniformly brown, with no other colouration, and minute conidia borne in long columns make Aspergillus terreus a distinctive species.
Images library
-
Title
Legend
-
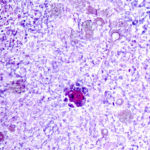
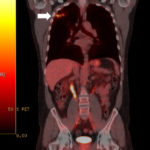
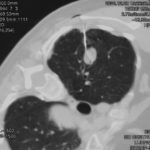
This 54 year old man developed right upper lobe shadowing after development of cough, chest pain and shortness of breath. He suffered from emphysema. Investigations, including a PET scan suggested carcinoma of the lung. He underwent an apical resection and histology showed bullae in the lung with one containing necrotic material and conidial heads consistent with Aspergillus.
Histology:
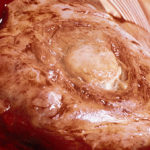
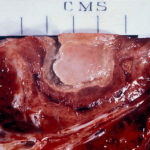
Two wedges of lung tissue were examined. The larger 90 x 35 x 35mm with adherent parietal pleura 100 x 45mm. Sectioning reveals irregular scarring and bullae in the lung tissue. No definite tumour is identified. A focus of possible necrosis up to 10mm in diameter is present, 10mm from the pleura and 20mm from the nearest staple line. Lung and adherent parietal pleura show dense fibrosis around a cavity (see fig A) arrow, lined by granulation tissue and fibrin. This is filled with necrotic material (Fig B) and branching septate fungal hyphae with conidial heads, consistent with Aspergillus and a fungal ball.(Fig C at higher power). A few scattered granulomata are seen away from the cavity. No invasion of lung parenchyma was seen. There is congestion of the lung parenchyma and collections of pigmented macrophages are seen within air spaces.Legends:
A- Section of lung showing a fungal ball within a cavity (x25). B- Showing branching septate hyphae with conidial heads (x250) C- Higher power magnification (x 500) showing the conidial heads more clearly. D – Edge of cavity showing from left to right – necrosis, granulaomatous reaction, fibrosis, chronic inflammation (x100). E- CT scan (July 08) showing a speculated nodular lesion in the right apex. F – Chest X-ray (May 08) – showing right upper lobe shadowing. G.PET scan (July 08)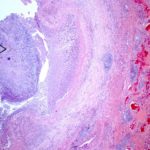 ,
,  ,
,  ,
,  ,
,  ,
,  ,
, 
-
Pt DB This patient with longstanding pulmonary disease developed Mycobacterium avium pulmonary infection which was treated. X rays in Jan 05 through to May 06 revealed an aspergilloma in upper right lobe cavity. Following a severe prolonged bout of coughing up black material- X rays on 22/9/07 showed a disappearance of the aspergilloma.( Images G & H). Go to case history
 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
, 
-
This 63 year old smoker presented with a new small mass in the right upper lobe. She had had tuberculosis as a teenager (1958) which recurred in 1962, requiring 2 long stays in a sanatorium. Since then she was well, until a new shadow was noticed on her chest X-ray. A CT showed a smooth round nodule, and to rule out carcinoma it was biopsied percutaneously. Histology showed fungal hyphae, consistent with Aspergillus , and serology confirmed infection with Aspergillus fumigatus. Following biopsy, an air fluid pocket has appeared, most consistent with an aspergilloma, as the lesion is solitary.
-
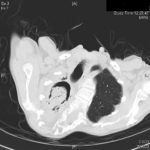
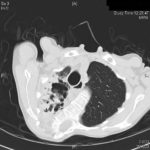
Patient MD with kyphoscoliosis and chronic cavitary pulmonary aspergillosis and an aspergilloma. Patient exhibited azole resistant A. fumigatus.
Further details
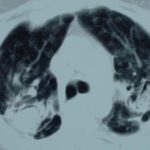
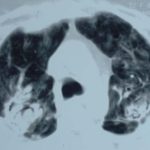
Image A. This CT scan cut shown shows a grossly distorted thorax because of the kyphoscoliosis, a nearly normal appearing left lung, her trachea at an odd angle, demonstrating the normal cartilage rings and an aspergilloma in a cavity which has replaced the right upper lobe. The cavity is surrounded by significant pleural thickening and fibrosis.
Image B. The other cut (slightly inferior) shows a complex large cavity and some smaller ones posteriorly, with some material consistent with a fungal ball within the large cavity. There is a separate cavity anteriorly and small air spaces within the extensive pleural thickening. Her trachea is widened. the left lung appears normal.
This patient with repaired juvenile scoliosis first recognised that she had pulmonary aspergillosis when she coughed up large amounts of blood, she was admitted to ICU and underwent bronchial artery embolisation, followed by tranexamic acid orally. A. fumigatus was cultured from sputum. A diagnosis of chronic cavitary pulmonary aspergillosis with an aspergilloma was made. She didn’t improve with itraconazole (no fall in Aspergillus precipitins and continuing symptoms, despite good blood levels) and was treated with voriconazole. She had a good sympomatic response, with marginal improvement in her Aspergillus precipitins titre. Remission continued for over 3 years but then her symptoms of cough and general fatigue returned. Her sputum grew A. fumigatus again, which had MICs to itraconazole (>8 mg/L, resistant), voriconazole (8mg/L, resistant) and posaconazole (2mg/mL, resistant). She is being treated with amphotericin B.
 ,
, 
-
Histopathological appearance of a fungus ball: it consists of a tangled mass of branching, septate hyphal with vesicular swellings in the center (H&E, x 200).

-
Further image details
Image A. Long standing sarcoidosis, on corticosteroids with fibrosis and cavitary disease, and a possible fungal ball in the cavity on the left (1996).
Image B. Long standing sarcoidosis, on corticosteroids with 2 cavities containing aspergillomas, one on the left and one on the right (1996).
Image C. Sarcoidosis with progressive cavity formation and aspergillomas. Probable CIPA given appearances (2000).
Image D. Sarcoidosis with progressive cavity formation and aspergillomas. Probable CIPA given appearances (2000).
Image E. Sarcoidosis with progressive cavity formation and aspergillomas. Probable CIPA given appearances (2000).
 ,
,  ,
,  ,
,  ,
,