Date: 7 May 2013
A four day A. fumigatus culture on malt extract agar (above). Light microscopy pictures are taken at 1000x mag., stained with lacto-phenol cotton blue (right).
Copyright:
With thanks to Niall Hamilton.
Notes:
Colonies on CYA 40-60 mm diam, plane or lightly wrinkled, low, dense and velutinous or with a sparse, floccose overgrowth; mycelium inconspicuous, white; conidial heads borne in a continuous, densely packed layer, Greyish Turquoise to Dark Turquoise (24-25E-F5); clear exudate sometimes produced in small amounts; reverse pale or greenish. Colonies on MEA 40-60 mm diam, similar to those on CYA but less dense and with conidia in duller colours (24-25E-F3); reverse uncoloured or greyish. Colonies on G25N less than 10 mm diam, sometimes only germination, of white mycelium. No growth at 5°C. At 37°C, colonies covering the available area, i.e. a whole Petri dish in 2 days from a single point inoculum, of similar appearance to those on CYA at 25°C, but with conidial columns longer and conidia darker, greenish grey to pure grey.
Conidiophores borne from surface hyphae, stipes 200-400 µm long, sometimes sinuous, with colourless, thin, smooth walls, enlarging gradually into pyriform vesicles; vesicles 20-30 µm diam, fertile over half or more of the enlarged area, bearing phialides only, the lateral ones characteristically bent so that the tips are approximately parallel to the stipe axis; phialides crowded, 6-8 µm long; conidia spherical to subspheroidal, 2.5-3.0 µm diam, with finely roughened or spinose walls, forming radiate heads at first, then well defined columns of conidia.
Distinctive features
This distinctive species can be recognised in the unopened Petri dish by its broad, velutinous, bluish colonies bearing characteristic, well defined columns of conidia. Growth at 37°C is exceptionally rapid. Conidial heads are also diagnostic: pyriform vesicles bear crowded phialides which bend to be roughly parallel to the stipe axis. Care should be exercised in handling cultures of this species.
Images library
-
Title
Legend
-
5 sputum samples were positive for A. niger, a bronchoscopy was normal and culture and microscopy were negative. Rx voriconazole, 200mg bd was given. An excellent clinical response was seen.
 ,
,  ,
,  ,
,  ,
, 
-
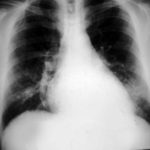
The patient was a 37-year old man in whom P.carinii pneumonia developed in August 1987, followed by esophageal candidiasis and upper gastrointestinal bleeding in September. Chronic perineal herpes led to the formation of rectourethral fistula and multiple episodes of urosepsis, for which he was given long-term ciprofloxacin therapy to suppress bacterial colonization of the bladder. He discontinued heavy alcohol use in September 1987 and smoked marijuana occasionally.On April 23 1989, the patient was admitted to the hospital with a two-month history of increasing dry cough with shortness of breath. He reported transient fever (temperature to 41°C). He was admitted with leukopenia, with his neutrophil count falling to 16 x 106/l on the second hospital day. A chest film showed bilateral fluffy lower-lobe infiltrates (this image). Zidovudine was discontinued. The patient had a rapidly downhill course despite intravenous treatment with trimethioprim-sulfamethoxazole. A bronchoscopy on the sixth hospital day revealed what appeared to be a foreign body in the left lower-lobe bronchus. It was removed, together with much necrotic, mucoid debris. On microscopic examination, the “foreign body” was necrotic, containing large numbers of hyphae and conidia in a manner typical of an aspegilloma or fungal cast. The culture grew A.fumigatus.
Clinical and radiologic improvement followed bronchoscopy, and itraconazole therapy was begun because of the concern about invasive aspergillosis in the setting of marked neutropenia. The patient tolerated the medication well at a dose of 200 mg twice daily, and the chest film became normal over the subsequent six weeks, after which itraconazole was discontinued. A sputum specimen cultured for fungus four weeks after the start of therapy was negative. After the initial improvement with itraconazole, the patient had recurrent urosepsis, associated with dehydration and marked confusion. Nine weeks after the discontinuation of itraconazole, he died of progressive dementia complicated by recurrent pneumonia and sepsis. There was no postmortem examination.
This patient was described (pt 11) and this chest radiograph reproduced in Denning DW, Follansbee S, Scolaro M, Norris S, Edelstein D, Stevens DA. Pulmonary Aspergillosis in the Acquired Immunodeficiency Syndrome. N Engl J Med 1991; 324: 654-662.
 ,
, 
-
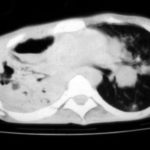
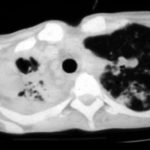
Image A. This 25 year old woman was previously well and presented with a pneumonia of uncertain aetiology. She has infiltrates in right upper-lobe and left middle and lower zones. The diagnosis was later made of chronic invasive pulmonary aspergillosis by bronchoscopy . Subsequently she was diagnosed with adult-onset chronic granulomatous disease with neutrophil function assays.
Image B. CT scan of the thorax just below the carina, showing almost complete opacification of the right lung and marked nodular shadowing around the hilum of the left lung.
Image C. Progression of pulmonary infiltrates are seen seven weeks later, despite administration of amphotericin B.
Image D. CT scan of the thorax above the carina showing near complete opacification of the right lung and multiple discrete nodular shadows in the left lung.
 ,
,  ,
,  ,
, 
-
02/10/09 X -ray shows improvement in appearances from initial presentation with complete chest radiographic resolution by 07/11/2008


![Asp[1]fumigatus](https://www.aspergillus.org.uk/wp-content/uploads/2013/11/Asp1fumigatus.jpg)
 ,
,  ,
,  ,
, 




