Date: 26 November 2013
cultures grown from BAL fluid showing formation of sclerotia.
Copyright:
Kindly donated by Dr Claudia Venturelli and Dr Giorgia Bertazzoni, Laboratory of Microbiology – Policlinico of Modena-Italy. © Fungal Research Trust
Notes:
These colonies were isolated from a BAL, (also with bacterial qrowth of S.aureus and S.maltophilia) from a patient with a VAP (undergoing corticosteroid treatment). The growth medium used is sabouraud dextrose agar , incubated at 37° C The identification is made by microscopic/macroscopic observation criteria.
Colonies on CYA 60-70 mm diam, plane, sparse to moderately dense, velutinous in marginal areas at least, often floccose centrally, sometimes deeply so; mycelium only conspicuous in floccose areas, white; conidial heads usually borne uniformly over the whole colony, but sparse or absent in areas of floccose growth or sclerotial production, characteristically Greyish Green to Olive Yellow (1-2B-E5-7), but sometimes pure Yellow (2-3A7-8), becoming greenish in age; sclerotia produced by about 50% of isolates, at first white, becoming deep reddish brown, density varying from inconspicuous to dominating colony appearance and almost entirely suppressing conidial production; exudate sometimes produced, clear, or reddish brown near sclerotia; reverse uncoloured or brown to reddish brown beneath sclerotia. Colonies on MEA 50-70 mm diam, similar to those on CYA although usually less dense. Colonies on G25N 25-40 mm diam, similar to those on CYA or more deeply floccose and with little conidial production, reverse pale to orange or salmon. No growth at 5°C. At 37°C, colonies usually 55-65 mm diam, similar to those on CYA at 25°C, but more velutinous, with olive conidia, and sometimes with more abundant sclerotia.
Sclerotia produced by some isolates, at first white, rapidly becoming hard and reddish brown to black, spherical, usually 400- 800 µm diam. Teleomorph not known. Conidiophores borne from subsurface or surface hyphae, stipes 400 µm to 1 mm or more long, colourless or pale brown, rough walled; vesicles spherical, 20-45 µm diam, fertile over three quarters of the surface, typically bearing both metulae and phialides, but in some isolates a proportion or even a majority of heads with phialides alone; metulae and phialides of similar size, 7-10 µm long; conidia spherical to subspheroidal, usually 3.5-5.0 µm diam, with relatively thin walls, finely roughened or, rarely, smooth.
Distinctive features
Aspergillus flavus is distinguished by rapid growth at both 25°C and 37°C, and a bright yellow green (or less commonly yellow) conidial colour. A. flavus produces conidia which are rather variable in shape and size, have relatively thin walls, and range from smooth to moderately rough, the majority being finely rough.
Images library
-
Title
Legend
-
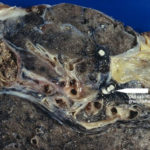
Macroscopic view medial aspect of left upper lobe of lung showing segmental collapse and congestion of lower segments, with mucus extruding from incised bronchi.
 ,
,  ,
,  ,
,  ,
, 
-
Born 75 years ago, Pt HK had 3 episodes of tuberculosis as a child and teenager, being treated with PAS and streptomycin. He suffered a ‘bad chest’ all his life and retired aged 54. Presenting with worsening and more frequent chest infections, he was referred with ‘bronchiectasis and Aspergillus sensitisation’. A diagnosis of chronic pulmonary aspergillosis was made in June 2009 on the basis of his chest radiograph and strongly positive Aspergillus precipitins (IgG antibodies) (titre 1/16). He also had Pseudomonas aeruginosa colonisation. His oxygen saturation was 87% and his pO2 6.8, pCO2 6.2 KPa.
His chest radiograph (see above, November 2009) was reported as showing; “ The lung fields are over-inflated. Bilateral apical fibrotic change secondary to old TB. No cavity seen.” At clinic, bilateral apical cavities were seen, with some associated pleural thickening at the left apex, without any evidence of a fungal ball.
He started posaconazole 400mg twice daily with therapeutic levels at subsequent visits. Sputum cultures never grew Aspergillus. Over the following 9 months he had no chest infections requiring antibiotics, his breathlessness worsened gradually and he remained easily fatigued. His Aspergillus antibody titres fell. Overall he felt better, but was concerned about declining respiratory status.