Date: 26 November 2013
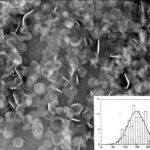
cultures grown from BAL fluid showing formation of sclerotia.
Copyright:
Kindly donated by Dr Claudia Venturelli and Dr Giorgia Bertazzoni, Laboratory of Microbiology – Policlinico of Modena-Italy. © Fungal Research Trust
Notes:
These colonies were isolated from a BAL, (also with bacterial qrowth of S.aureus and S.maltophilia) from a patient with a VAP (undergoing corticosteroid treatment). The growth medium used is sabouraud dextrose agar , incubated at 37° C The identification is made by microscopic/macroscopic observation criteria.
Colonies on CYA 60-70 mm diam, plane, sparse to moderately dense, velutinous in marginal areas at least, often floccose centrally, sometimes deeply so; mycelium only conspicuous in floccose areas, white; conidial heads usually borne uniformly over the whole colony, but sparse or absent in areas of floccose growth or sclerotial production, characteristically Greyish Green to Olive Yellow (1-2B-E5-7), but sometimes pure Yellow (2-3A7-8), becoming greenish in age; sclerotia produced by about 50% of isolates, at first white, becoming deep reddish brown, density varying from inconspicuous to dominating colony appearance and almost entirely suppressing conidial production; exudate sometimes produced, clear, or reddish brown near sclerotia; reverse uncoloured or brown to reddish brown beneath sclerotia. Colonies on MEA 50-70 mm diam, similar to those on CYA although usually less dense. Colonies on G25N 25-40 mm diam, similar to those on CYA or more deeply floccose and with little conidial production, reverse pale to orange or salmon. No growth at 5°C. At 37°C, colonies usually 55-65 mm diam, similar to those on CYA at 25°C, but more velutinous, with olive conidia, and sometimes with more abundant sclerotia.
Sclerotia produced by some isolates, at first white, rapidly becoming hard and reddish brown to black, spherical, usually 400- 800 µm diam. Teleomorph not known. Conidiophores borne from subsurface or surface hyphae, stipes 400 µm to 1 mm or more long, colourless or pale brown, rough walled; vesicles spherical, 20-45 µm diam, fertile over three quarters of the surface, typically bearing both metulae and phialides, but in some isolates a proportion or even a majority of heads with phialides alone; metulae and phialides of similar size, 7-10 µm long; conidia spherical to subspheroidal, usually 3.5-5.0 µm diam, with relatively thin walls, finely roughened or, rarely, smooth.
Distinctive features
Aspergillus flavus is distinguished by rapid growth at both 25°C and 37°C, and a bright yellow green (or less commonly yellow) conidial colour. A. flavus produces conidia which are rather variable in shape and size, have relatively thin walls, and range from smooth to moderately rough, the majority being finely rough.
Images library
-
Title
Legend
-
Itraconazole rash – macropopular rash after 7 days treatment with Itraconazole, in a patient with AIDS

-
A 72 year-old male patient had been in treatment for many years for severe asthma with relatively good exercise tolerance. Over the past two years he had increasing problems of shortness of breath, cough and productive sputum. There was no history of chest pain, haemoptysis or fever. His total IgE was 680.0 IU/l, and specific IgE against Aspergillus fumigatus was 14.6 IU/l. Precipitins against A. fumigatus were weakly positive (titre 1/2), and there was no eosinophilia. Computed tomography revealed marked emphysema but only mild bronchiectasis. Based on these results he was diagnosed with severe asthma with fungal sensitisation (SAFS) and itraconazole was started (SporanoxTM 200mg bds). Itraconazole dosage was reduced to 200 mg daily one month later due to progressive bilateral ankle oedema. Itraconazole levels by bioassay were 17.5 mg/l at that time (normal range 5-15 mg/l). Despite showing improvement on his chest symptoms, peripheral oedema became a major negative impact on patient’s quality of life. There were no signs of heart failure. Figure 1 was taken 2 months after itraconazole was started, when drug levels were 9.8 mg/l. Itraconazole was replaced by voriconazole. Concomitant medications included furosemide (80 mg daily) and spironolactone (100 mg daily). After discontinuing itraconazole, the oedema quickly subsided.
Ankle oedema is an uncommon complication of therapy with itraconazole. It has occurred in about 4% of patients treated in clinical trials involving this drug. This complication seems to be more frequent in patients concomitantly receiving calcium channel blockers, which was not the case for our patient. The mechanism is unknown. It usually does not represent cardiac failure, another reported side effect of itraconazole, but this must be excluded. Marked oedema requiring drug suspension is a rare phenomenon, and has not been previously reported in association with itraconazole.
 ,
,  ,
, 
-
The insert shows the size of the discs. These discs dissociate after infusion to release amphotericin B preferentially into the reticuloendothelial system and lung. This form of amphotericin B is marketed as either Amphotec or Amphocil, depending on the country.