Date: 26 November 2013
This 24-year-old male with AML on chemotherapy developed recent onset fever and cough. A: Chest radiograph showing patchy air space consolidation involving both lungs.
Copyright:
With thanks to Dr Sanjay Sharma, Dept Radiodiagnosis , All India institute of Medical Sciences , New Delhi 110 029 India .
Notes:
This patient was proven to have airway invasive aspergillosis. Though similar appearances can be caused by active tubercular/ viral bronchiolitis and even aspiration pneumonia.
Images library
-
Title
Legend
-
PtDS2 –Repeated chest infections arrested by itraconazole therapy in ABPA and bronchiectasis
DS2 developed asthma age 24 and now aged 62. From about age 30 she started getting repeated chest infections and a few years later ABPA and bronchiectasis was diagnosed. Infections continued requiring multiple courses of antibiotics annually. At one point DS2 developed a pneumothorax, possibly because of excess coughing. She has chronic rhinitis and mannose binding lectin deficiency. In May 2011, she started itraconazole therapy, and has needed no antibiotic courses for her chest since. Her rhinitis with sinusitis occasionally bothers her. She is delighted to have gone 18 months with no chest infections.
 ,
,  ,
, 
-
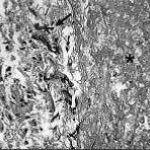
Aspergillus hyphae (arrow) in the lumen without invasion of the necrotic bronchial wall (*) (Nicod 2001).
-
fibrinonecrotic material (arrow) from the airway shown in A, with subocclusion of the bronchial lumen (*)
-
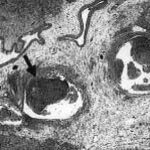
Fibrinous or pseudomembranous bronchitis (arrow) with subocclusion of the airways (* indicates subocclusion of the airways by pseudomembranes)

-
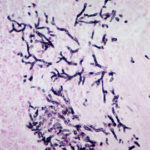
Bronchoscopic biopsy demonstrated septate hyphae with branching at 45o (methenamine silver stain ×400).