Aspergillus was the etiologic agent in 24% of cases of fungal endocarditis (FE) reported in English language indexed medical journals (or between 0.25% and 2.5% of all infectious endocarditis) (Ellis, 2001). Most cases of Aspergillus endocarditis (AE) involve adults but children and at least one neonate have been described (Luke 1963; Barst, 1981; Mourier, 2009). In a case series of patients between 2003 and 2009 the ages ranged between 8 months and 75 years with 37% being in their fifties (McCormack, 2010).
In this series males outnumbered females: 26 cases versus 8. More than twice as many cases of FE are caused by Candida spp. as by Aspergillus spp. – a figure that has remained constant over the last 30 years. This is perhaps surprising, given the relative increase in invasive aspergillosis compared to candidiasis in immunocompromised patients. FE, including AE, has been extensively reviewed in a meta-analysis (Ellis, 2001) and AE has been reviewed in a more recent series of cases (McCormack, 2010).
There are some identifiable pre-requisites for developing FE and AE. Valvular anatomic abnormalities were seen in 64% of patients with FE (eg previous valve surgery, rheumatic heart disease, previous bacterial endocarditis) (Ellis, 2001). In the more recent case series of AE, 74% of patients had previous surgery, 21% had no surgery and two patients had either a pacemaker or defibrillator in situ (McCormack, 2010). Of the 25 patients with prior surgery 48% had heart valve surgery but 20% had other cardiac surgery and 32% had non-cardiac surgery. In this series 40% had a history of recent transplant surgery of various organs. Conditions that predispose to invasive fungal infections (eg malignancy, antimicrobial use, neutropenia, injecting drug use and immunosuppressive states and therapy) are also commonly found in AE.
These factors are dynamic with a changing contribution in recent years: vascular lines, non-cardiac surgery, immunocompromise, injecting drug use and allergic bronchopulmonary aspergillosis or asthma (treated with corticosteroids) are becoming increasingly common. In one cluster of 4 cases of AE an environmental airborne source was suspected (Mehta, 1990) but most cases are sporadic. Complex combinations of risk factors are frequently found in patients with AE.
Diagnosis of AE is difficult and frequently delayed: the diagnosis was made post-mortem in 16% of cases (McCormack, 2010). Blood cultures are almost always negative. Mycological examination of vegetations or emboli is the most common means of diagnosis. Galactomannan testing was positive in 4 out of 9 cases: from serum in 3 cases and from bronchoalveolar lavage fluid in one. Polymerase chain reaction (PCR) testing was positive in 6 out of 6 cases: 5 from serum and one from vegetation tissue (McCormack, 2010). Fever, changing/new heart murmurs, major peripheral embolisation (particularly femoral and cerebral), focal or generalised neurologic features, heart failure and dyspnoea are the most common clinical features.
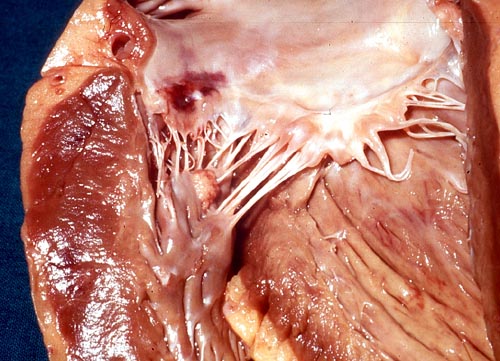
In the case series of AE 15% of patients presented with a new murmur and 38% presented with an embolus (McCormack, 2010). Of 35 cases of AE 14 involved the aortic valve, 14 the mitral valve, 5 the tricuspid valve and 2 were mixed (McCormack, 2010). Classical signs such as digital clubbing, Osler’s nodes and splenomegaly are uncommon. Therefore the diagnosis of AE is often delayed or misdiagnosed as bacterial endocarditis, fever of unknown origin or stroke. The diagnosis should be suspected particularly in a middle aged man with a history of a prior valvular abnormality or recent surgery, who presents with fever, major peripheral emboli or neuro-embolic phenomena. The presence of large bulky vegetations on echocardiography should further heighten the suspicion, although not all patients have large lesions.
Crude mortality from FE in general is around 72% although in recent years this has dropped to around 59%. For AE the mortality rate was 68% (McCormack, 2010). The cause of death is directly attributable to Aspergillus in 90% of cases and is usually due to catastrophic valvular failure or complications secondary to major embolic phenomena: usually cerebral.
Neither valve replacement nor anti-fungal drug treatment alone impact significantly on outcome from AE (Denning, 1990; Gumbo, 2000; Ellis, 2001). The median duration of survival from time of first treatment for AE was only 11 days, compared to 690 days for Candida endocarditis (Ellis, 2001). Of 8 patients (32% of the total case series: McCormack, 2010) who survived from AE 7 had valve surgery (Ryu, 2009; Brili, 2009; Badiee, 2009); Saxena, 2007; Vassiloyanakopoulos, 2006; Reis, 2005; Cook 2004). One patient, an 8 month old girl who developed AE following a liver transplant for biliary atresia, survived following AE with antifungal therapy and no surgery (Mourier, 2009). There have been only 1 or 2 cases described in the world literature where a successful outcome with medical therapy alone has been documented. Surgical intervention is frequently undertaken when a complication of AE has occurred, or a trial of antifungal therapy has failed. Surgical intervention should be embarked upon earlier than is usually the case.
Amphotericin B has historically been the most frequently used antifungal drug in AE. This drug’s high toxicity profile, particularly nephrotoxicity, along with poor penetration into cardiac vegetations, limit it’s efficacy in AE. Of 22 patients treated for AE liposomal amphotericin B at a dose of 3 or 5 mg/kg/day was used in 7 out of the 8 survivors; combined with other antifungals in 3 of these. The other patient received voriconazole alone. All patients treated with conventional amphotericin B or itraconazole died. There was no clear advantage in using combinations of antifungals (McCormack, 2010) although such therapy requires further study. The minimum duration of initial antifungal therapy should be 4 weeks, longer periods may be required if the response is slow or complications develop. Since survival rates are so poor, very little data are available on recurrence of AE. Since Candida endocarditis recurs in 30% of survivors, sometimes years after the initial presumptive cure, it would be prudent to have an active follow up program for survivors of AE. Secondary prophylaxis with voriconazole for at least 2 years, possibly lifelong in some cases, is recommended (McCormack, 2010).
Delay in diagnosis and delayed surgical intervention are commonly encountered in the management of AE. Heightened clinical diagnostic acumen, use of sensitive serological diagnostic tests, early valve replacement and a maximum tolerated dose of a lipid based amphotericin B preparation should form the basic management strategy for this serious infection.
Images
March 2010
Joe McCormack
Associate Professor of Medicine and Director of Infectious Diseases
The University of Queensland School of Medicine
Mater Clinical School,
Department of Medicine & Infectious Diseases,
First Floor Whitty Building,
Raymond Terrace,
South Brisbane QLD 4101
Australia
j.mccormack1@uq.edu.au
joe.mccormack@mater.org.au
References:
Case histories:
Aspergillus endocarditis following aortic valve replacement (48)