- Jan 1729
- Jan 1789
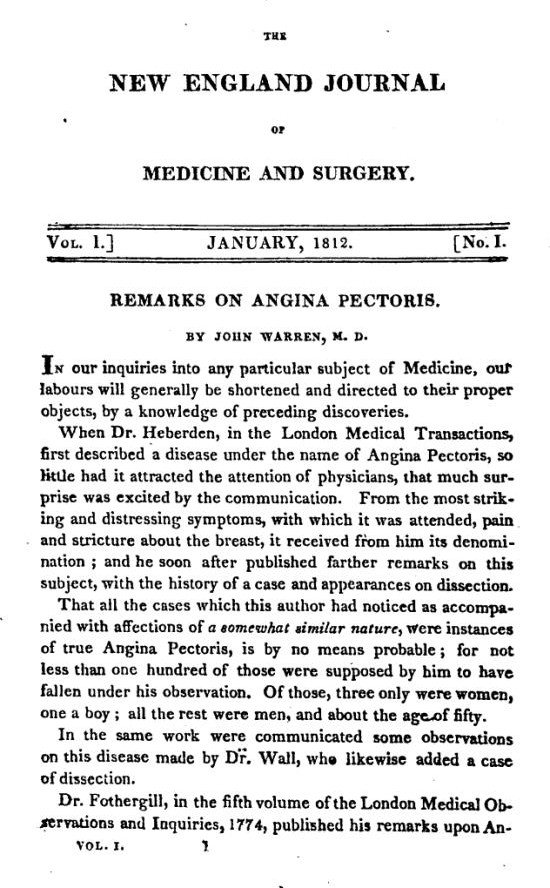
- Jan 1812
- Jan 1812
- Apr 1812
- Jan 1842
- Aug 1861
- Jan 1863
- Aug 1863
- Jul 1868
- Nov 1868
- Aug 1871
- Aug 1871
- Dec 1871
- Dec 1871
- Mar 1872
- Jun 1873
- Jul 1874
- Dec 1876
- Feb 1879
- Mar 1882
- Aug 1882
- Jan 1944
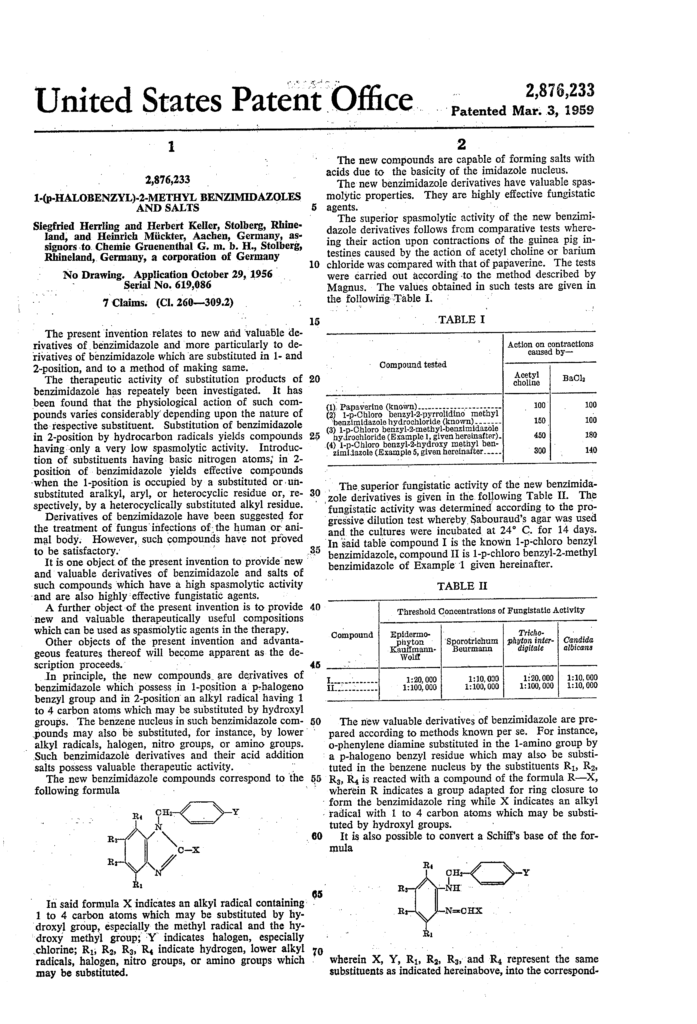
- Mar 1959
- Sep 1960
- Jan 1964
- Jan 1969
- Jan 1971
- Nov 1977
- Jan 1979
- Feb 1979
- Apr 1979
- Jan 1981
- Jan 1987
- Jan 1992
- May 2002
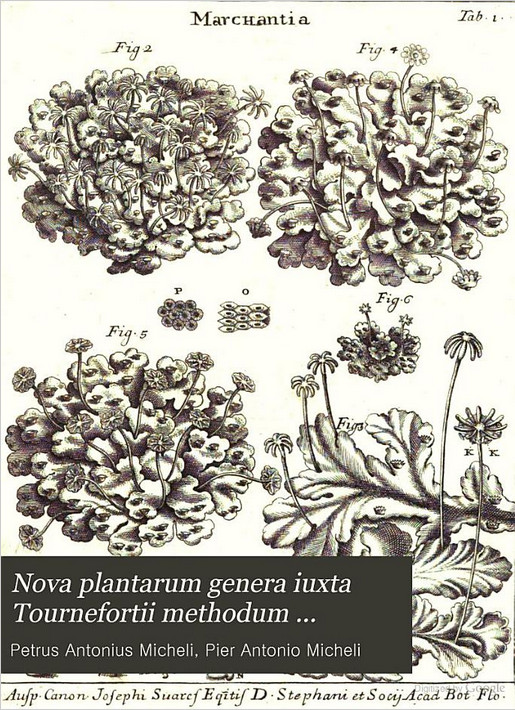
First description of Aspergillus
Aspergillus first described in Nova plantarum genera by Pier Antonio Micheli. Nova plantarum genera (Florentiae) 1729), is an illustrated work detailing some 1900 ‘plant’ species, the majority previously not having been described scientifically. Of these about 900 were in fact fungi or lichenised fungi.
Discovery of Aspergillus as a Human Pathogen
In the midst of the 1789 French Revolution, Jacques Thibault, a 22 year old soldier experienced severe facial pain with the elevation of his cheekbone and the protrusion of his right eye. When physicians perforated Thibault’s alveolar process, a fungal mass was found in the maxillary sinus. Resection could not be performed due to excessive bleeding. Twenty-two days later, the fungal mass had grown and filled part of his mouth and his entire right nostril, causing difficulty in swallowing and breathing.
Thibault was admitted to a Paris Hospital where the fungal mass was excised by a surgeon and white heat cautery was applied to destroy any remnants of the fungus. Small fungal growths reappeared three to four weeks later at the back of the sinus and the soft palate; all were cauterized using a branding iron. Mr. Thibault left the hospital 134 days after admission with no subsequent recurrences.
Thibault’s case was the first recorded infection attributed to Aspergillus.
References
Barnes E. A short history of invasive aspergillosis, 1920 to 1965. The Aspergillus Website. (www.aspergillus.org.uk).
Bennett JH. On the parasitic vegetable structures found growing in living animals. Transactions of the Royal Society of Edinburgh 1842;15:277-294.
Brakhage AA, Schmidt AJB. Georg W. Fresenius and the Description of the Species Aspergillus fumigatus. Contributions to Microbiology 1999;2:I-4. [PubMed]
Plaignaud, M. Observation concerning a fungus in the maxillary sinus. Journal de Chirugie 1791;87:244-251.
Flannigan B, et al. Microorganisms in home and indoor work environments. Aspergillus Image Bank (www.aspergillus.org.uk).
Wind of Cannon Balls
..thus modified, several times with success. Med. and Phys. Journal. Wind of Cannon Balls. Mr. Ellis has published an interesting paper in the Edinburgh Medical and Surgical Journal, ” on the accidents ascribed to the wind of a ball.” He has adduced many instances to prove that these accidents are not imaginary…
First mention of the Plague
An Essay on the disease called Yellow Fever, with observations concerning Febrile Contagion, Typhus Fever, Dysentery, and the Plague, partly delivered as the Guletonian Lectures, before the College of Physicians, in the years 1806 and 1807 (first mention of the Plague)
The earliest description of pulmonary aspergillosis
The earliest description of pulmonary aspergillosis was published in 1842 by physician, John H. Bennett. Bennett noted the presence of a fungus in the lungs of a post mortem patient with pneumothorax. The fungus was described as “Numerous jointed transparent tubes, here matted together, there isolated…mingled with round or oval corpuscles, which, however, were larger and more developed.”
References
Barnes E. A short history of invasive aspergillosis, 1920 to 1965. The Aspergillus Website. (www.aspergillus.org.uk).
Bennett JH. On the parasitic vegetable structures found growing in living animals. Transactions of the Royal Society of Edinburgh 1842;15:277-294.
Brakhage AA, Schmidt AJB. Georg W. Fresenius and the Description of the Species Aspergillus fumigatus. Contributions to Microbiology 1999;2:I-4. [PubMed]
Researches of Pasteur Respecting the Theory of Spontaneous Generation
…growths which appeared, were the same as in flasks exposed to the open air, viz.: of infusoria, bacterium, of muccdines the penicilium, ascopkora, aspergillus and some others. When calcined asbestos alone was introduced, no vegetation appeared. It was thus demonstrated that among the dust suspended in ordinary…
Aspergillus species fumigatus first described.
In 1863 the species fumigatus was first described by physician Georg W. Fresenius. “From my studies of isolates obtained from human lung infections… I had the chance to learn more about this fascinating species of Aspergillus…. The species we describe here is very different to A. glaucus and also from all other [Aspergillus] species which have been described so far.” Fresenius named the new species A. fumigatus. He observed that the spores had a green pigmentation and had no septated fertile hyphae or conidiophores. Fumigatus is derived from Latin “fumigave” which means smoky referring to the smoky blue-gray mycelium.
Subsequent cases of Aspergillus infections over the next several years showed the most frequent species of Aspergillus responsible for human infection was A. fumigatus. From 1920 to 1965, cases of disseminated aspergillus infections were implicated in the heart and CNS in addition to the sinuses and lungs. Potassium iodide was used as therapy from the start of the twentieth century until the end of World War II. In the 1940s, sulphonamides and the new “wonder drugs” of antibacterial agents were used to treat fungal infections with inconsistent results. The discovery and formulation of nystatin and amphotericin in the 1950’s led to the first effective antifungal agents against Aspergillosis.
References
Barnes E. A short history of invasive aspergillosis, 1920 to 1965. The Aspergillus Website. (www.aspergillus.org.uk).
Brakhage AA, Schmidt AJB. Georg W. Fresenius and the Description of the Species Aspergillus fumigatus. Contributions to Microbiology 1999;2:I-4. [PubMed]
Plaignaud, M. Observation concerning a fungus in the maxillary sinus. Journal de Chirugie 1791;87:244-251.
On Mycetoma …
…MYCETOMA. By H. V. Carter, M.D. Lond. Assistant-Surgeon Bombay Army. In the following remarks it is proposed to give some account of a very serious disease widely prevailing in India, and in its nature and pathological characters well worthy the attention of the surgeon and naturalist. “Mycetoma” stands…Aspergillus growing on the membrane of the tympanum
…5th. The secretion of urine is slightly, that of saliva markedly, increased.–1 bid. Mushrooms in the Ear.–Two new kinds of mushrooms of the Aspergillus order, growing on the membrane of the tympanum, are described by Dr. C Robin, in a paper read to the French Academy of Sciences. This parasitical..
A Parasitic Growth in the External Auditory Meatus
…manubrium injected. By the strong injection of warm water, several white membranous substances removed, which by microscope showed filaments of the Aspergillus mixed with epithelium and debris ; none of the fructifying heads were found. July 3d.–Both membranas tympani apparently clean ; injection of vesselsl…‘all the fungi lie found at Jena, viz.: Penicillium, Aspergillus’
Editorials and Medical Intelligence
…llallier’s cultures with kincpock lymph, sown upon different substrata, and have obtained all the fungi lie found at Jena, viz.: Penicillium, Aspergillus, the bastard forms between these two fungi, Mucor Oidium and a TomÃn, together with Micrococci, Cryptococci and Arthrococci;and have seen under…‘white growth appeared at the outer portion of the moatus’
…persisted for about three months, at the end of which time a white growth appeared at the outer portion of the moatus, continuous with the growth of aspergillus further in. The microscope revealed a thick network of mycelium, resembling that of Penicillium glaucuni Leukhardtii, interspersed with oval brown…Parasitic Growths in the External Meatus
…the Penicillium paucum and Aspergillus frlaucus are well known, he has not been able, notwithstanding the most careful examination, to detect in any one of his fourteen cases either a pure bastard example of Penicillium, or one resulting from copulation with Aspergillus.It is with reference to this…‘in connection with the earlier crop of Aspergillus’
…vorablo to the development of Penicillium, and subsequently in connection with the earlier crop of Aspergillus, of a bastard growth. The second case is a comparatively simple one. C. D. aged 08, a carpenter by trade, presented himself at the aural clinic of the Mass. Char. Eye and Ear Infirmary in May…Case of Morbid Condition of the Umbilical Cord
…cultivation, to throw light on this point. Halber considers the favus plant to be anaspergillus, other authorities have thought it to be other well-known moulds. Recent investigators will traco it back to either the aspergillus or penicillium. On the other hand, they have never succeeded in growing it from…‘case of alarming haemorrhago following the removal of a small polypus’
…case of alarming haemorrhago following the removal of a small polypus from the short process of the incus ; a case of exuberant development ofaspergillus, without any symptoms of irritation. The third article, by Dr. Moos, on the significance of tho higher musical tones, gives the histories of several…On the Germ Theory of Disease
…of the disease. Salisbury admits that he has found, associated with the palmolla, other cryptogams, belonging to genera, Torula, Penicillium, Aspergillus, Sphserotheca, in the urine of ague patients; but these he regards as accidental. Tho palmolla may have been equally accidental. The strongest confirmatory…
Recent Progress in Dermatology (Aspergillus)
Recent Progress in Dermatology
…appropriating its 1 Extrait du Discours d’Installation. Annules do Dermatologie et de Sypbiligraphie, tome vil. No. 4. nutriment. Attempts to inoculate aspergillus glaueus and penicillium glaucum upon animals failed, and these moulds have, in the author’s opinion, no connection with these affections. Tinea…Recent Progress in the Treatment of Children’s Diseases
…Dark grayish membranous formations are sometimes seen firmly adherent to the drum membrane. Under the microscope they prove to be a fungus, — the aspergillus glaucus. Linear perforations are caused by sudden compressions of air, as boxing the ear. Large losses of substance are due to suppurative inflammations…‘occupying himself with the larger fungi, — such as aspergillus’
…of the immunity following exposure to the influences of poison by inoculation or otherwise. Occupying himself with the larger fungi, — such as aspergillus and penicillium, whose spores are several hundred times the size of a micrococcus, — he obtained results which he made the subject of a paper in…‘aspergillus fumigatus and flavescens, without any acclimatization at all are capable of killing’
…Lichtheim, of Berne, who have shown: Firstly, that penicillium cultivated purely and inoculated is innocuous ; secondly, that certain mould fungi, aspergillus fumigatus and flavescens, without any acclimatization at all are capable of killing animals when inoculated, in the same way, and with the same anatomical…First antifungal activity of an azole compound
Woolley DW. Some biological effects produced by benzimidazole and their reversal by purines. J Biol Chem 1944; 152: 225–32.
Development of Chlormidazole
In 1952, Jerchel et al. revived Woolley’s work and reported that certain substituted benzimidazole compounds had significant antifungal activity. This publication encouraged other investigators to screen this group of chemicals in search of a clinically useful antifungal agent. The breakthrough came in 1958 to 1959 when chlormidazole, a chlorobenzyl imidazole, was developed and studied in clinical trials. Chlormidazole was sold as a 5% topical cream, the first azole derivative developed and marketed as an antifungal drug.
References
Seeliger, H. P. R. 1958. Pilzemmende Wirkung eines neuen Benzimidazol Derivatives. Mykosen 1:162-171.
Herrling, S., H. Sous, W. Kruppe, G. Osterloh, and H. Muckter. 1959. Experimentelle Untersuchungenuber eine neue gegen Pilze wirksame Verbindung. Arneim. Forsch. 9:489-494.
Guido Pontecorvo Letters
Guido Pontecorvo and Prof Haldane exchange letters and discuss the work of Haldane’s colleague S K Roy and Pontecorvo’s decision to ask Roy to give a seminar at Glasgow. He also mentions that at Glasgow the main purpose of his research work is “genetics analysis via somatic segregation and gives an update on his Aspergillus work, to which Haldane responds “you are certainly going for Everest rather than Ben Lomond”.
Papers taken from the Wellcome Library Archives
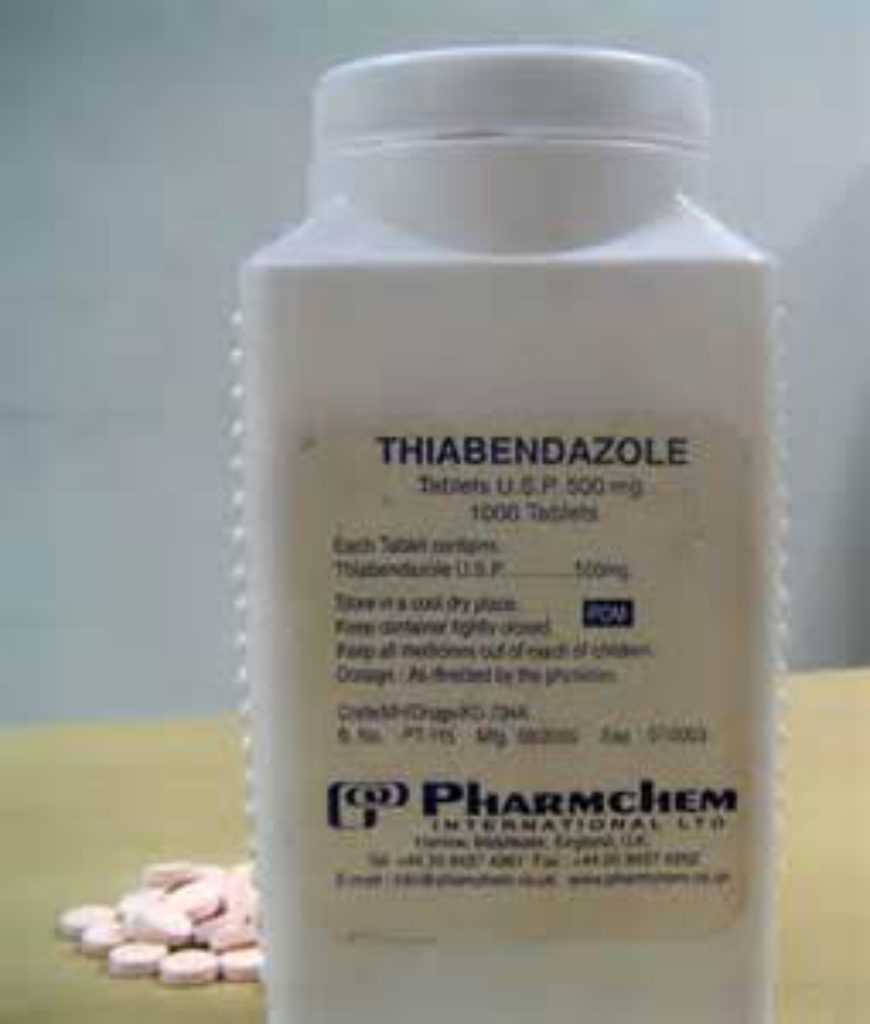
Antimycotic properties of thiabendazole
With the introduction of chlormidazole, interest in the antifungal activity of azole compounds began to increase. For example, after the introduction of thiabendazole, a thiazolyl-benzimidazole, in 1961 by Merck Sharp & Dohme for use as a broad-spectrum antihelminthic drug, Robinson et al. tested the compound for antifungal activity in vitro. It was effective against many dermatophytes and Aspergillus species, but since its activity against yeast-like fungi was minimal, the compound was not developed as an antifungal agent.
Thiabendazole, was first discovered to be an unusually potent broad spectrum anthelmintic. Extensive acute and chronic toxicity studies in a variety of animal species have shown thiabendazole to be well tolerated even when administered orally over a 2-year period. More recently thiabendazole was discovered to suppress the growth of saprophytic fungi. The present paper deals with the effect of thiabendazole in vitro on various pathogenic and saprophytic fungi. Included in the latter group of organisms are cultures which are known to produce mycotoxins. Comparative studies were made with nystatin and griseofulvin.
Reference
Robinson, H. J., H. F. Phares, and 0. E. Graessle. Antimycotic properties of thiabendazole. 1964.. J. Invest. Dermatol. 42:479-482.
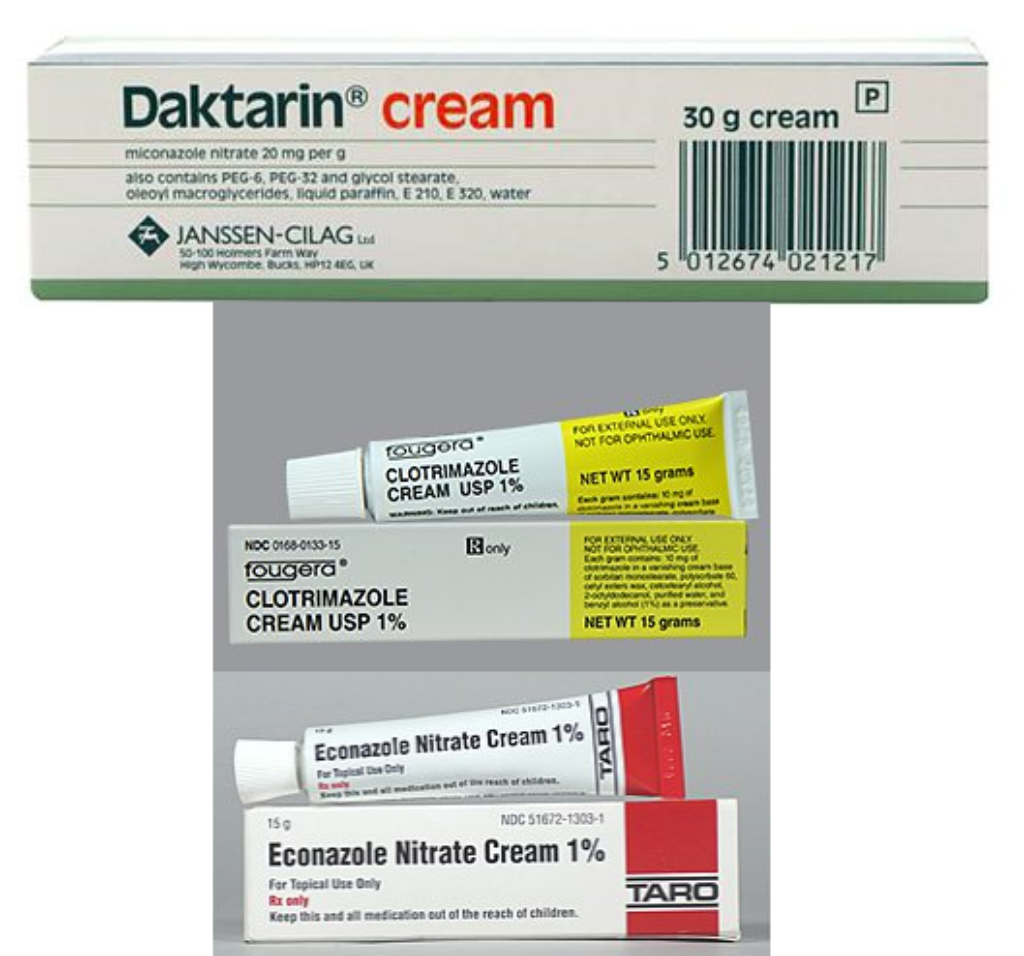
Clotrimazole developed by Bayer AG, Miconazole and Econazole by Janssen Pharmaceutica
In the late 1960s, three compounds from two different laboratories were introduced in the literature; these drugs firmly established azoles as antifungal agents. Clotrimazole, developed by Bayer AG (Wuppertal, Federal Republic of Germany), and miconazole and econazole, developed by Janssen Pharmaceutica, were introduced within months of each other. This era of azole antifungal compounds was so new and competitive that the less descriptive report of clotrimazole antifungal activity was published 3 years prior to the more detailed description of the chemical synthesis. These three imidazoles continue to be used today for treatment of fungal infections, demonstrating the success of these early discoveries. Unfortunately, their use also reveals the slow evolution of the azole class of antifungal drugs during the past two decades.
References
Plempel, M., K. Bartmann, K.-H. Buchel, and E. Regel. 1969. Experimentelle Befunde uber einneues oral wirksames Antimykoticum mitbreiten Wirkungsspecktrum. Dtsch. Med. Wochenschr. 94:1356-1364.
*Excerpt from Fromtling RA. Overview of medically important antifungal azole derivatives. Clin Microbiol Rev. 1988 Apr;1(2):187-217.
Antifungal activity found in mebendazole.
Mebendazole, a benzoyl-benzimidazole developed by Janssen Pharmaceutica (Beerse, Belgium) in 1973 as a broad-spectrum antihelminthic agent, was shown to have antifungal activity. Despite the fact that the antifungal activity of these two compounds was not pursued, the data supported the concept that two azole compounds had potential as antifungal drugs for human use.
Reference
Brugmans, J. P., D. C. Thienpont, I. van Wongaarden, 0. F. VanparUs, V. L. Schulmans, and H. L. Lauwers. 1971. Mebendazole in enterobiasis. J. Am. Med. Assoc. 217:313-316.
*Excerpt from Fromtling RA. Overview of medically important antifungal azole derivatives. Clin Microbiol Rev. 1988 Apr;1(2):187-217.
Discovery of Butaconazole
Butoconazole is an antifungal imidazole developed for the treatment of vaginal candidiasis by Syntex Research Laboratories (Palo Alto, Calif.). The synthesis and initial antifungal properties of this compound were first reported in 1978. Butoconazole has a broad spectrum of antifungal activity, including clinically important yeasts and dermatophytes. The antifungal activity of butoconazole was comparable to ketoconazole, with the exception that ketoconazole was superior against Aspergillus species.
This antifungal cream is currently used to mainly treat Candida infections of the vagina.
Discovery of Oxiconazole
Oxiconazole is an antifungal imidazole jointly developed by F. Hoffmann-LaRoche and Siegfried AG, both of Basel, Switzerland. It only has moderate activity against Aspergillus and is marketed for the treatment of dermatomycoses and vaginal candidiasis (Sochynsky and Hardcastle [ed.], Pharma Projects, p. a 299, May 1986).
Original paper: Mixich, G., and K. Thiele. 1979. Ein Beitrag zur stereospezifischen Synthese von antimykotisch wirksamen Imidazolyloximathern. Oxiconazol-nitrat (Sgd 301-76), ein neues Breitbandantimykotikum. Arneim. Forsch. 29:1510-1513.
Discovery of Ketoconazole
Ketoconazole was the first available drug for the oral treatment of systemic fungal infections.
Miconazole, econazole, and clotrimazole are potent broad-spectrum antimycotics which show high in vitro activity against almost all fungi of clinical interest. They have also been successfully applied for topical use in many clinical trials, particularly in mucocutaneous candidosis of the vagina and in dermatophytosis. The major disadvantage of miconazole, econazole, and clotrimazole is that serum, urine, and body fluid levels after oral doses are disappointingly low, at best hardly sufficient to inhibit fungal growths. In some cases, however, intravenous miconazole therapy can be successfully applied for the treatment of systemic fungal infections. in In this paper, we report the synthesis and antifungal properties of ketoconazole (I), a new 1,3-di~xolanylmethylimidazole derivative, which is at present undergoing clinical investigation.
* excerpt from Original paper
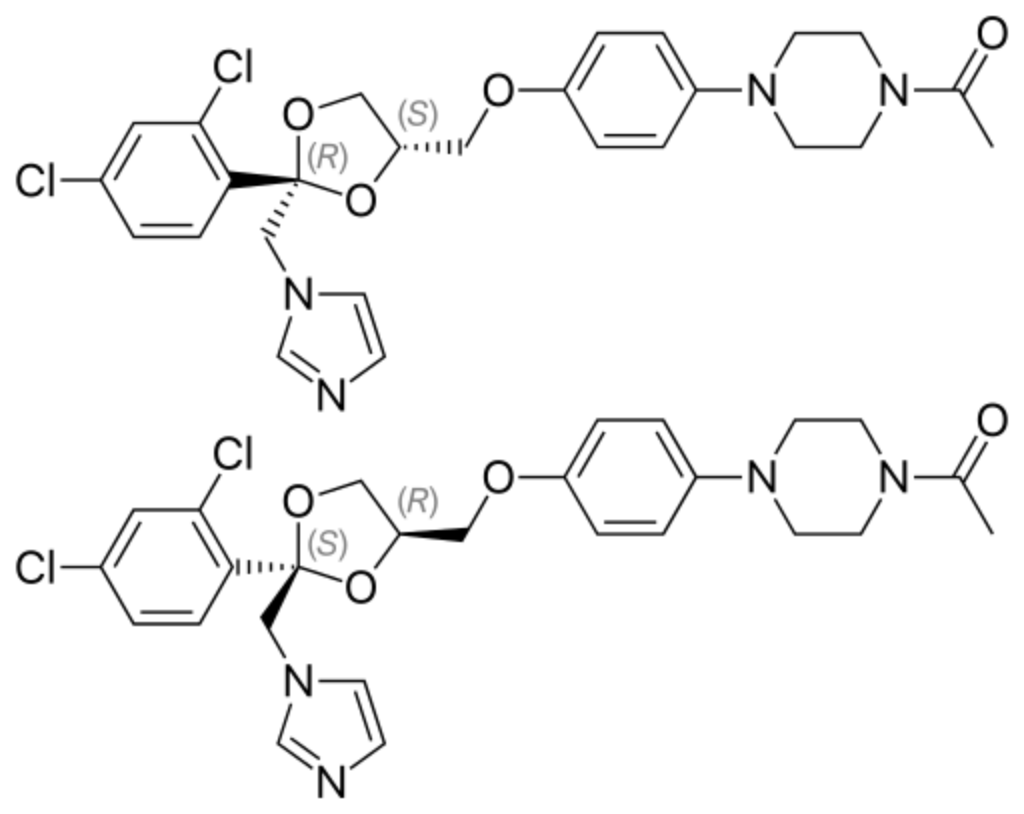
Discovery of Tioconazole
Tioconazole is a 1-substituted imidazole derivative synthesized and developed by Pfizer U.K. (Sandwich, England). Tioconazole has broad-spectrum in vitro inhibitory activity against a variety of pathogenic yeasts, dermatophytes, and Aspergillus species, as well as activity against some chlamydia, trichomonads, and gram-positive bacteria (53). It is indicated for the topical therapy of superficial dermatophytic and yeast infections of the skin and for vaginal candidiasis. In the United States, tioconazole has been approved for over the counter use in the treatment of skin and nail infections due to dermatophytes and yeasts, including those infections complicated by gram-positive organisms (Sochynsky and Hardcastle (ed.), Pharma Projects, p. a 301, May 1986).
*Excerpt from Fromtling RA. Overview of medically important antifungal azole derivatives. Clin Microbiol Rev. 1988 Apr;1(2):187-217.
Discovery of Fluconazole
Fluconazole is a first-generation triazole antifungal medication. It differs from earlier azole antifungals (such as ketoconazole) in that its structure contains a triazole ring instead of an imidazole ring. While the imidazole antifungals are mainly used topically, fluconazole and certain other triazole antifungals are preferred when systemic treatment is required because of their improved safety and predictable absorption when administered orally. Fluconazole is an antifungal medication used for a number of fungal infections.This includes candidiasis, blastomycosis, coccidiodomycosis, cryptococcosis, histoplasmosis, dermatophytosis, pityriasis versicolor and occasionally aspergillosis. It is also used to prevent candidiasis in those who are at high risk such as following organ transplantation, low birth weight babies, and those with low blood neutrophil counts. It is given either by mouth or by injection into a vein. Reference Henderson, J. T. 1987. Fluconazole-a significant advance in the management of human fungal disease, p. 77-79. In R. A. Fromtling (ed.), Recent trends in the discovery, development and evaluation of antifungal agents. J. R. Prous Publishers, Barcelona.
Discovery of D-0870 (ICI 195739)
ICI 195,739 reduces ergosterol biosynthesis by inhibiting sterol C-14 demethylation, resulting in the accumulation of methylated sterols (K. Barrett-Bee, J. Lees, J. Campbell, P. Pinder, and L. Newboult, First Int. Conf. Drug Res. Immunol. Infect. Dis. Antifungal Drugs: Synthesis, Preclin. Clin. Eval., abstr. no. 17, 1987; K. Barrett-Bee, J. Lees, J. Campbell, P. Pinder, and L. Newboult, Proc. N.Y. Acad. Sci in Press)
This is similar to other antifungal azole derivatives; however, the inhibition of ergosterol synthesis by ICI 195,739 occurs at drug concentrations that are much less than those that induce a reduction in cholesterol biosynthesis, suggesting that this compound will not adversely affect mammalian enzyme systems.*
D0870 reached phase 1 clinical trials but unfortunately use for treating fungal infection was discontinued in 1995 when an adverse event occurred in an HIV patient and subsequent analysis showed that its pharmacokinetics were unpredictable.
References
*Excerpt from Fromtling RA. Overview of medically important antifungal azole derivatives. Clin Microbiol Rev. 1988 Apr;1(2):187-217.
Denning DW, Hall L, Jackson M, Hollis S. Efficacy of D0870 compared with those of itraconazole and amphotericin B in two murine models of invasive aspergillosis. Antimicrob Agents Chemother. 1995 Aug;39(8):1809-14.
Venkateswarlu K, Denning DW, Kelly SL. In-vitro activity of D0870, a new triazole antifungal drug, in comparison with fluconazole and itraconazole against Aspergillus fumigatus and Candida krusei. J Antimicrob Chemother. 1997 Jun;39(6):731-6.
Keith J. Williams and David W. Denning* Termination of development of D0870. J Antimicrob Chemother 2001; 47:720-721
Discovery of Itraconazole
Developed as an alternative to ketoconazole by Janssen Pharmaceutica, itraconazole showed good activity against Aspergillus, much better than ketoconazole and it was approved for use in the US in 1992.
Excerpt from Wikipedia:
Itraconazole has a broader spectrum of activity than fluconazole (but not as broad as voriconazole or posaconazole). In particular, it is active against Aspergillus, which fluconazole is not. It is also licensed for use in blastomycosis, sporotrichosis, histoplasmosis, and onychomycosis. Itraconazole is over 99% protein-bound and has virtually no penetration into cerebrospinal fluid. Therefore, it should not be used to treat meningitis or other central nervous system infections.[8] According to the Johns Hopkins Abx Guide, it has “negligible CSF penetration, however treatment has been successful for cryptococcal and coccidioidal meningitis”.[9]
It is also prescribed for systemic infections, such as aspergillosis, candidiasis, and cryptococcosis, where other antifungal drugs are inappropriate or ineffective.
Itraconazole has also recently been explored as an anticancer agent for patients with basal cell carcinoma, non-small cell lung cancer, and prostate cancer.[10]
Voriconazole Approved for Use
Developed by Pfizer Limited, voriconazole (first marketed as vFend) is a triazole and is highly active against Aspergillus infection, also used to treat candidiasis, coccidioidomycosis, histoplasmosis, penicilliosis, and infections by Scedosporium or Fusarium. Available orally or via injection voriconazole is approved for primary treatment for acute invasive aspergillosis by the US FDA and for the treatment of adults and children with invasive aspergillosis aged over 2 years in Europe.
First studied in humans in 1991.
References
Vfend (Voriconazole for intravenous injection), NDA 21-267, Background Document for Antiviral Drug Products Advisory Committee Meeting, 4 October 2001. Pfizer Inc. [online]. Available from URL: www.fda.gov/ohrms/dockets/ac/0…