In 1925, Van and colleagues described a remarkable frequency (50%) of mould skin sensitivity in Dutch asthmatics principally to Mucor, Penicillium and Aspergillus spp [i]. In 1928 both Hansen [ii] in Germany and Jimenez-Diaz [iii] with colleagues reported positive skin tests to crude extracts of fungi.
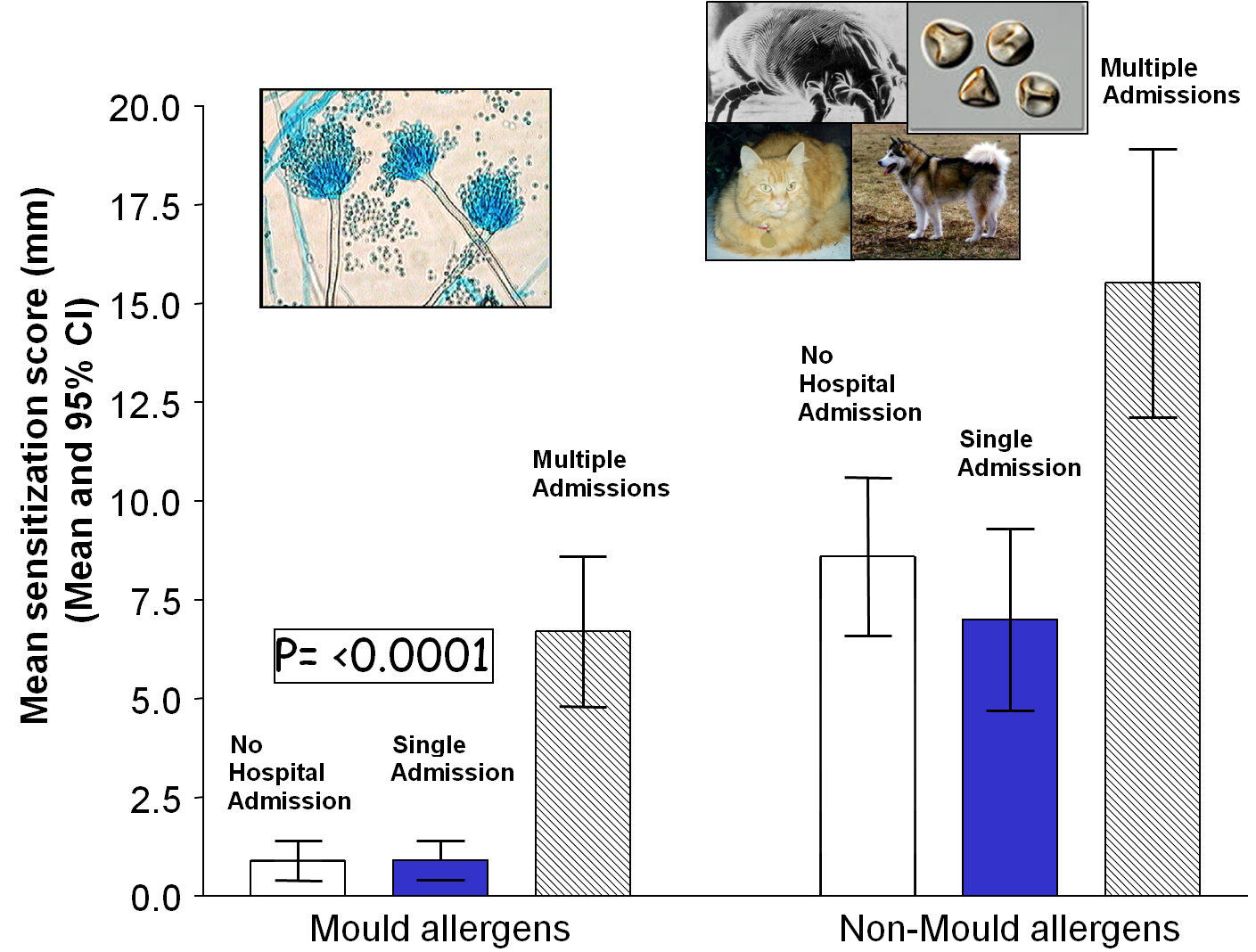
The European Community Respiratory Health Survey showed 36% of with asthma had one or more positive skin prick tests, defining that person as atopic. Of these, 4.4% were sensitized to Alternaria and 2.3% were sensitised to Cladosporium compared with 21% sensitized to house dust mite, 17% sensitized to grass pollen and 10% sensitized to cat. Fungal sensitisation is much less common than other sensitisations in the general population in Europe, but more common in those with severe asthma.
Link with severe asthma
Fungal sensitisation is more prevalent in people with severe asthma. Approximately 25% of adult asthma patients referred to specialists and up to 75% of patients with severe asthma requiring multiple hospital admissions are sensitized to one or more fungi[iv]. Patients with severe asthma and fungal sensitization have SAFS
Issues with skin tests
Unfortunately reagents from different manufacturers differ and give slightly different skin prick test results in different people. Skin test responses may vary over time in the same individual even if performed in an identical manner with the same reagent. Asthma may also ‘go through good and bad periods’, possibly consistent with this. While the correlation between positive skin tests and IgE RAST test on blood is reasonable, there is enough discordance to require both to be done to identify all patients who are sensitized to fungi. Skin tests tend to be more sensitive. Some clinics test for a wide range of fungal sensitivity, others test for a limited number or only for Aspergillus fumigatussensitivity. A reasonable minimum testing set is A. fumigatus, Candida albicans, Cladosporium herbarum, Alternaria alternata, Penicillium chrysogenum (notatum) and Trichophyton mentagrophytes.
An example of skin prick testing on the arm showing positive reactions to the positive control (histamine), and negative reaction to the negative control. Positive reactions to house dust mite (D pteronysinus), cat, grass and Cladosporium. A positive reaction is a raised area at least 3mm in diameter.


Another example of skin allergy testing showing a reaction to the positive control (+, histamine) and to grasses. The ‘cat’ reaction was less than <33mm, the criteria for a positive result.
The following video demonstrates the technique of skin testing for all types of allergen including fungal.
IgE testing
Fungal allergy is partly mediated through IgE binding to mast cells leading to histamine release, recognized as immediate-type hypersensitivity. Delayed-type hypersensitivity is not mediated through IgE, but eosinophils and possibly basophils appear to be important mediators of inflammation. IgE can directed at a specific fungus and/or the total IgE can be elevated. A key diagnostic criterion of ABPA is an elevated total serum IgE. Different cut-off levels have been identified or proposed for different conditions, and may also vary by test manufacturer. Commercial assays for total IgE are ALercheck,inc; abcam; Cortez diagnostics, Elabscience, Aviva systems;Siemens; Thermo Scientific.
A detectable Aspergillus specific IgE is another key diagnostic criterion ABPA (and allergicAspergillus sinusitis) and defines Aspergillus sensitization which is associated with reduced lung function in cystic fibrosis, chronic obstructive pulmonary disease and following pulmonary tuberculosis. Immediate skin prick tests against Aspergillus (see more), also detect Aspergillus IgE, but there is imperfect concordance between serum detection of Aspergillus IgE and skin testing.
|
ABPA marker |
Europe |
India |
|
|
Adult asthma |
Adult CF |
Adult asthma |
|
|
Aspergillus IgE |
detectable |
>5.7 kUA/L |
>1.91 kUA/L |
|
Total IgE |
>1,000 kIU/L |
>185 kIU/L |
>2347 IU/mL |
Many different fungi, and other allergens, can induce sensitization. Fungal sensitisation in childhood (especially Alternaria) is associated with persistent asthma later in life. Elevated fungal specific IgE is one of the diagnostic criterion for SAFS, and may be elevated in fungal rhinosinusitis. Fungal-specific serum assays are available from Thermo-Fisher and Siemens. Skin prick testing for fungal-specific immediate hypersensitivity (or IgE) also defines fungal sensitisation.
[i] Van Leeuwen WS, Nien Z, Kremer, W, Varenkamp H. Ztschr Immunitatsforsch 1925;44:1.
[ii] Hansen K. Uber schimmelpilz-asthma. Verhandl Deutsch Gesellsch Inn Med 1928;40:204.
[iii] Jimenez-Diaz C, Sanchez Cuenca B, Puig J. Climatic asthmas. J Allergy 1932;3:396-403.
[iv] O’Driscoll BR, Hopkinson LC, Denning DW. Mold sensitization is common amongst patients with severe asthma requiring multiple hospital admissions. BMCPulm Med. 2005;5:4.
