Submitted by MeganB on 19 July 2018
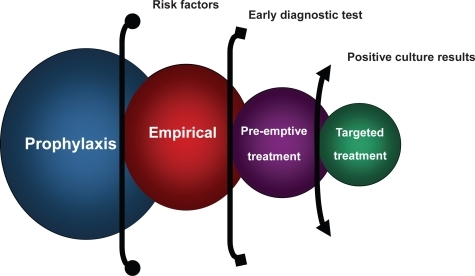
Invasive fungal infections present a significant risk to cancer patients, with early diagnosis and aggressive antifungal treatment proving key to survival. Though great advances have been made in recent years, the diagnosis of invasive fungal infections continues to be challenging, with the current approach being the prescription of prophylactic empirical antifungal therapy to those cancer patients deemed to be at high risk for fungal infection. This approach can lead to the treatment of many cancer patients with antifungal drugs who later experience will tell us had no fungal infection. This treatment strategy can be associated with prolonged hospitalisation, higher costs and an increase in adverse effects (something antifungal drugs are very prone to).
A recent study by MarÍa E. Santolaya and colleagues in Chile investigated the efficacy of pre-emptive antifungal therapy in comparison to empirical treatment when administered to high-risk paediatric cancer patients.
High-risk patients were defined as those diagnosed with a specified risk factor, in addition to febrile neutropenia, and were randomised to receive either empirical or pre-emptive therapy. The pre-emptive group received antifungal treatment only if the febrile neutropenia was accompanied by clinical, laboratory, imaging or microbiological pre-defined criteria suggesting the presence of an invasive fungal infection and this applied to 42% of the group.
The evaluation for the purpose of diagnosing a fungal infection included ANC, absolute monocyte count (AMC), CRP, repeat blood cultures, serum GM, chest and sinus CT scan, abdominal ultrasound and other imaging studies and diagnostic evaluations according to clinical presentation [fundoscopy, echocardiography, MRI, bronchoalveolar lavage (BAL), skin or other tissue biopsy].
 With regard to mortality rates, the results show that pre-emptive therapy was just as effective as an empirical therapy in treating high-risk paediatric cancer patients. Importantly, pre-emptive therapy also significantly reduced the use of the aggressive antifungal treatments, which present further complications and costs. Therefore, this approach to antifungal therapy in cancer patients may be an improvement on current procedures.
With regard to mortality rates, the results show that pre-emptive therapy was just as effective as an empirical therapy in treating high-risk paediatric cancer patients. Importantly, pre-emptive therapy also significantly reduced the use of the aggressive antifungal treatments, which present further complications and costs. Therefore, this approach to antifungal therapy in cancer patients may be an improvement on current procedures.
Unfortunately, there are still significant challenges to face when adopting this method, such as the heavy reliance on complex diagnostic laboratory support. The authors recommend the prior implementation of non-culture based diagnostic techniques into clinical practice. This, together with the active monitoring of patients, would lay the foundations for the introduction of evidence-based pre-emptive antifungal therapy in high-risk cancer patients.
News archives
-
Title
Date