Submitted by GAtherton on 6 December 2016
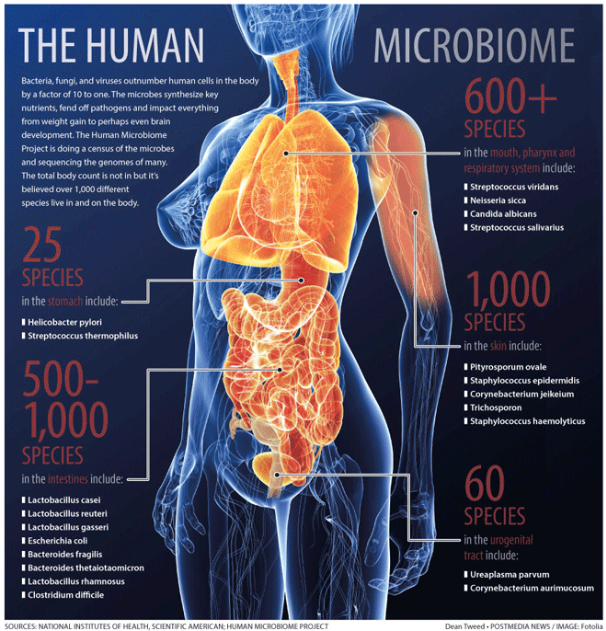
The study of the microbes that inhabit our skin and mucosa is rapidly revealing new information on our relationship with those we carry around and their relationship with us and our health. In a recent article by Kong in Dermatology Times Dr Kong highlights a study carried out in 2013 on patients who are prone to fungal infections as they have a primary genetic immunodeficiency.
Those patients had higher numbers of Aspergillus and Candida in parts of their microbiome compared with normal controls and their skin harboured bacteria that were unique to this group of people. The suggestion is that their immune deficiency allows different microbes to grow on their skin and that those microbes are less good at competing out fungal growth compared with the bacteria that normally live on our skin so the fungi can get a foothold and start to colonise much more than they would on a normal host and that leads to a greater vulnerability to fungal infection.
Sounds a bit odd? Instead of focusing on the presence of a pathogenic microbe and removing it by washing or disinfecting, microbiome research suggests that we might still remove the pathogens but we must then take care to re-establish the growth of microbial colonisers (or find a way that they can be preserved while removing the pathogen) that are normally present on the skin of healthy people in order to prevent future infection. A few years ago we would have simply sterilised the area, leaving it open to being colonized by pathogens. Cleanliness is not necessarily the next best thing to Godliness after all.
NB while you are thinking about the impact that this way of thinking about our microbial friends and infection, have a read of the article our image came from. It describes the amazing differences made to gut disorders by this research.
This TEDtalk is also an eye-opener!
News archives
-
Title
Date