Submitted by BethBradshaw on 26 July 2018
Very rarely, fungal rhinosinusitis (aspergillosis/mucormycosis) can spread via blood vessels from the mucosa lining the sinuses to the brain, skull base and eye socket. Even with surgery and antifungal therapy mortality rates of 50-80% have been reported, with the risk of death being related to the extent of spread. This can take from a few days to up to 4 weeks.
Dr Ignacio Javier Fernandez and colleagues in Bologna (Italy) reviewed the charts of 1832 at-risk (immunocompromised) patients, and found 19 that had been affected by invasive fungal rhinosinusitis (IFRS). Before 2007, the average time delay before treatment was just over 12 days and the mortality rate was 43%. In 2007, the centre introduced an early diagnosis protocol that reduced the average delay to around 5 days and increased the mortality rate to 17%. The degree of disease progression was strikingly lower after introduction of the early diagnosis protocol: 42% of cases did not progress beyond the nose, and no cases progressed to the intracranial form.
EORTC guidelines require a diagnosis of IFRS to be confirmed by histological and microbiological testing, but the authors suggest that a combination of clinical, radiological, serological and endoscopic data can give a diagnosis that is reliable enough to proceed with surgery.
They describe nasal endoscopy as the key test, with signs including mucosal ischaemia and plain necrotic areas with a blackish/grayish color, crusting, and absence of bleeding upon scraping, commonly located in the region of the middle turbinate, ethmoid, or septum.
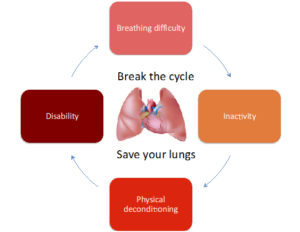
The authors provided the early diagnosis protocol in the form of a flowchart (below) that could be implemented in other high-risk settings such as haematology wards or transplant centres.

News archives
-
Title
Date